Drug-coated balloon catheter(DCB) is a new treatment strategy for coronary artery disease, which is mostly used for the treatment of in-stent restenosis (ISR) after bare-metal stents and drug-eluting stents. Recent studies have shown that DCB has good efficacy and safety in patients with small vessel disease and high risk of bleeding. Recently, the international DCB consensus group released the latest guidelines on the use of DCB in coronary artery disease, focusing on the new indications and emerging technologies of DCB.
Coronary stents can reduce restenosis and prevent acute occlusion after balloon angioplasty. The application of dual antiplatelet therapy (DAPT) provides more favorable acute outcomes and lower restenosis rate than angioplasty alone. Drug-eluting stents (DES) can reduce ISR by continuously releasing drugs that inhibit intimal hyperplasia. However, even the second generation des has the problems of late-onset atherosclerosis and thrombosis events (such as stent thrombosis). The application of DCB can reduce this risk.
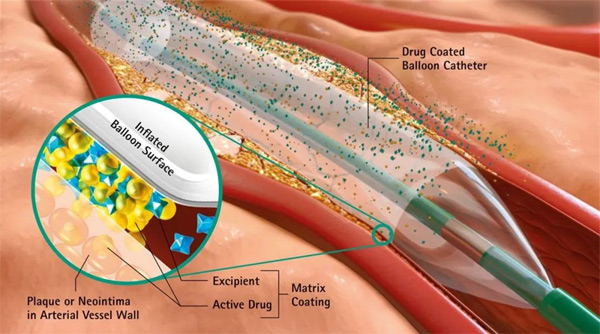
After angioplasty, negative vascular remodeling and neointimal hyperplasia can lead to restenosis. These processes are often slow and can be prevented by the sustained release of drugs that inhibit endometrial hyperplasia. Although different coatings were tested on the balloon catheter, local administration of paclitaxel eventually showed a significant reduction in the incidence of restenosis, an important aspect of which was positive remodeling.
Recently, sirolimus and its derivatives have been used in the study of DCB. Compared with paclitaxel, the transfer rate of sirolimus and its derivatives is poor and needs to be retained in tissues for a long time. At present, several local balloon-based administration methods of sirolimus and its derivatives have been proposed. In the preclinical model, the biological effect of using zotamox instead of paclitaxel coating was confirmed. The saber trial reports the first clinical experience of sirolimus delivered via a porous balloon in the treatment of coronary artery ISR. In the desired trial, paclitaxel-coated and sirolimus coated balloon groups had similar late lumen loss within 6 months and no difference in clinical events within 12 months.
At present, paclitaxel is still the first choice for DCB, and the conventional dose is 2 ~ 3.5μg /mm2. Different coating formulation and coating technology can bring different pharmacokinetic characteristics, which is one of the key factors for successful drug transfer. Therefore, the interaction among drug dosage, preparation, release kinetics and lesion seem to be the key to the vascular response after DCB treatment.
For uncomplicated lesions, it is recommended to use hemispheric saccule or non-compliant balloon with the same diameter as the artery. In the case of expected vessel filling or potential insufficient size and difficult balloon delivery, we can start with a smaller balloon and reassess the vessel size after the use of vasodilators. If the standard semi-compliant balloon fails to expand, a high-pressure noncompliant balloon or cutting balloon is recommended.
If calcification is present in the vessel wall, the use of these special balloons may produce more predictable and uniform pre-expansion results than standard balloons. For ISR patients, positive pre-expansion with a high-pressure balloon may be recommended to solve the serious problem of insufficient stent expansion. Besides, adjuvant treatment of lesion pretreatment, such as rotary milling, laser track rotary cutting, lithotripsy or prolonging dilation time, can promote the smooth progress of balloon angioplasty and subsequent drug treatment.
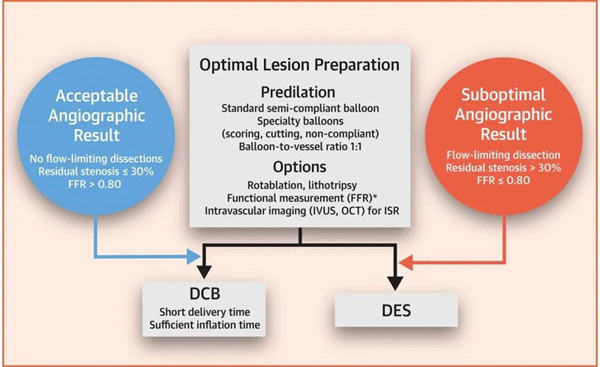
Once the lesion has been pretreated, the best results of balloon angioplasty should be confirmed before the delivery of DCB, including the following factors: (1) a balloon that can be completely expanded and its size is consistent with the diameter of the artery; (2) residual stenosis≤30%; (3) TIMI blood flow grade 3; (4) no blood flow restriction, i.e. angiography must exclude vascular lumen, wall and any anatomy Delayed contrast agent clearance in the plane.
FFR is recommended to define functional outcomes in patients with acute lumen enlargement after pre-dilation, residual stenosis, and angiographic limitations. After two years of follow-up, FFR>0.90 showed that the improvement rate of angioplasty was lower than that of the previous two years. However, recent studies have shown that the optimal cut-off value of FFR after balloon angioplasty is set at 0.85 or even 0.75 to predict future outcomes. Despite the lack of valid data on the ideal FFR threshold after conventional balloon angioplasty, an FFR of 0.80 may be a good compromise for guiding angioplasty. This problem needs further study.
The transportability of the first generation DCB is lower than that of the standard balloon with larger cross-section, and the transportability of the contemporary DCB is improved. The recently used pre-dilated balloon can be used as a guide, but distal lesions, extreme tortuosity or excessive calcification may lead to DCB delivery failure. The catheter with good support, extensible guide, auxiliary wire and deep finger guide tube can be used as the choice of balloon transportation.
Before DAPT, balloon angioplasty for coronary artery disease was not widely used due to short-term and long-term adverse outcomes. Recently published randomized controlled study data show that DCB technology has the advantages of optimal lesion pretreatment, functional detection, inhibition of intimal hyperplasia, short-term DAPT, and has become an effective choice for the treatment of coronary artery disease in most clinical situations.
